It’s not a big secret. Social determinants — where people are born, live, learn, work, play, worship, and age significantly impacts many aspects of health, including quality of life outcomes and risks of future health issues. Just take a look at some recent headlines:
“Research Highlights the Impact of Social Determinants of Health on Hypertension Control.”
“Social Determinants of Health Associated with Asthma Morbidity in Children.”
“Addressing Social Determinants of Health Has a Huge Impact.”
These are real headlines for just three of many articles discussing the impact of social determinants of health (SDOH) — all released within days of each other.
Social determinants and the impact on population health
The impact of SDOH on overall population health became so overwhelmingly evident that the U.S. Department of Health and Human Services included a goal specifically related to SDOH in its Healthy People initiative: “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”
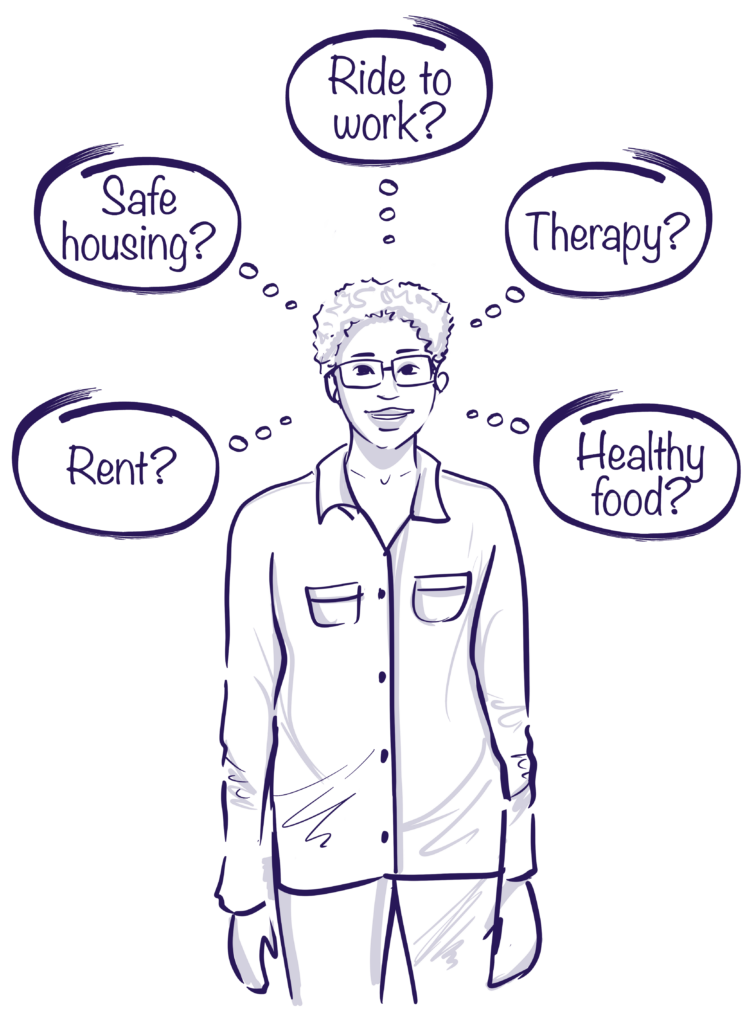
Addressing SDOH means far more than promoting healthy choices, which is an oversimplified and incomplete understanding of how social determinants impact health. SDOH are the sum of the environmental conditions a person faces on a daily basis, and in many cases, these factors are beyond any one individual’s control. And collectively — across years — these social determinants have a cumulative effect on health, one that is disproportionately negative for many underserved populations.
While the healthcare industry has much left to learn about how social determinants impact individual and population health and how it can most effectively address these effects, one thing is clear. SDOH are often not choices, healthy or otherwise. Public health organizations, educators, and leaders in transportation and housing play a pivotal role in improving those environmental conditions, and thus they play a key role in reducing the health disparities that are a result of SDOH.
Shifting industry attention spotlights social determinants
For a long time, the healthcare industry was — for better or worse — almost solely focused on the amount and type of care provided. This was evident in the fee-for-service payment model. Then, in 2001, the Institute of Medicine published Crossing the Quality Chasm, which shed light on safety gaps across the industry. In response, a plethora of quality-focused measures, programs, departments, and even entire organizations were created.
Then, the shift to value-based care further shed light on the need to improve the quality of care delivered. However, that model still places the majority of attention on clinical outcomes. Despite efforts to focus on safety and quality, people as a whole are not healthier, and racial and ethnic disparities persist. But as more research into SDOH surfaces, the impact these determinants have on overall health has grown apparent.
The statistics are sobering: as much as 80% of health outcomes are non-clinical. Socioeconomic factors like education, job status, and income; health environment; health behaviors like tobacco use and diet; and access to high-quality care all form the basis for a person’s health. For instance, patients with unstable housing are 4x more likely to be readmitted after receiving hospital care.
Since 2020, we’ve also learned that the COVID-19 pandemic further exacerbated health equity gaps, with 79% of Black patients hospitalized for COVID-19 compared to just 19% of white patients. In addition, the COVID-19 mortality rate for Black, Latino, and Pacific Islander patients is 2 to 2.6x that of white patients. These disparities are estimated to reverse more than 10 years of progress made in closing the life expectancy gap between Black and white people.
Although there is little doubt that addressing SDOH is important for improving population health, it has been traditionally difficult for organizations to place funding behind SDOH initiatives because measuring the impact is challenging. Billions are spent each year on community benefit programs, including SDOH-specific programs, but few have documented long-term outcomes, and many organizations struggle to scale and expand even when efforts are successful. Meanwhile, Medicaid and uninsured patient costs continue to rise.
Even so, there is some progress. CMS has proposed several new health equity and maternal health quality measures. These include Hospital Commitment to Health Equity; Screening for Social Drivers of Health; Screen Positive Rate for Social Drivers of Health; among others. Just last month, CMS announced its Maternity Care Action Plan in support of the Biden-Harris Administration’s Blueprint for Addressing the Maternal Health Crisis. These developments are a start, but there’s more work to be done.
Screening for social determinants can help improve outcomes
As the appetite for more data-driven solutions that address SDOH increases, tools that allow healthcare organizations to digitally enable and scale staff are important elements to any initiative. GetWell Navigate integrates two-way messaging, automated outreach and workflows, SDOH survey collection, and seamless coordination across teams.
Our AI-driven solution autonomously engages patients to:
- Screen for SDOH needs over time
- Navigate patients to hospital or community resources
- Capture longitudinal risk
- Boost routine care
- Escalate patients with complex needs or clinical risks
In particular, the ability to screen for SDOH needs allows organizations to assess patients for those non-clinical factors that disproportionately affect health. Does the patient lack access to healthy food? Do they feel unsafe at home?
More than just a standard-issue texting solution, GetWell Navigate pulls from information collected from patient records and couples that with the SDOH screener to create a 360-degree profile of a patient. Recommendations and information are not generically produced and disseminated to a large patient population. Instead, based on what we know about a patient — everything from health history to geographic location, work status, and level of access to care — we can provide resources that are not just useful but also actionable.
Establishing this connection and rapport is invaluable. According to the Commonwealth Fund, U.S. adults are the least likely in the world to have a regular physician or place of care, or a longstanding relationship with a primary care provider.
To effectively bridge this gap, programs intended to address SDOH are most likely to be successful when combining high-tech innovation with the high-touch element of an actual person. One way Get Well does this is through our GetWell Navigators, who are trained to screen patients for SDOH concerns, including any mental health needs a person may have. They serve as advocates, and, importantly, act as relationship builders.
Asking questions about a patient’s non-clinical needs enables providers to stay ahead of potential clinical issues. When this type of information is relayed, appropriate resources can be deployed, potentially preventing future health issues. This can also help patients following an episode of care — an important benefit, given that many patients don’t understand discharge instructions due to health literacy or language barriers.
The Navigators work to build trust and provide users with a person they can turn to when they have questions or need additional information. By providing personalized support and communicating with patients on their terms, the Navigators deliver a level of care that is more likely to keep patients coming back. As trust transitions into loyalty, patients are more likely to remain with a provider or within a system because they feel like access to the resources they need is convenient and that the information is valuable.
The bottom line
There is little doubt that addressing SDOH can help improve both individual and population health. Questions begin to arise when trying to determine how to do so in a cost-effective manner that demonstrates meaningful improvements in outcomes.
Combining technology that enables organizations to scale resources while layering in a human element that allows for empathetic, bi-directional communication gives organizations the ability to meet needs all around. The real bottom line is that patients are people and they want — and deserve — to be treated as such. Technology can bring you to the finish line, but it’s true people-centered care that leverages that technology in smart ways that will help you cross it.
